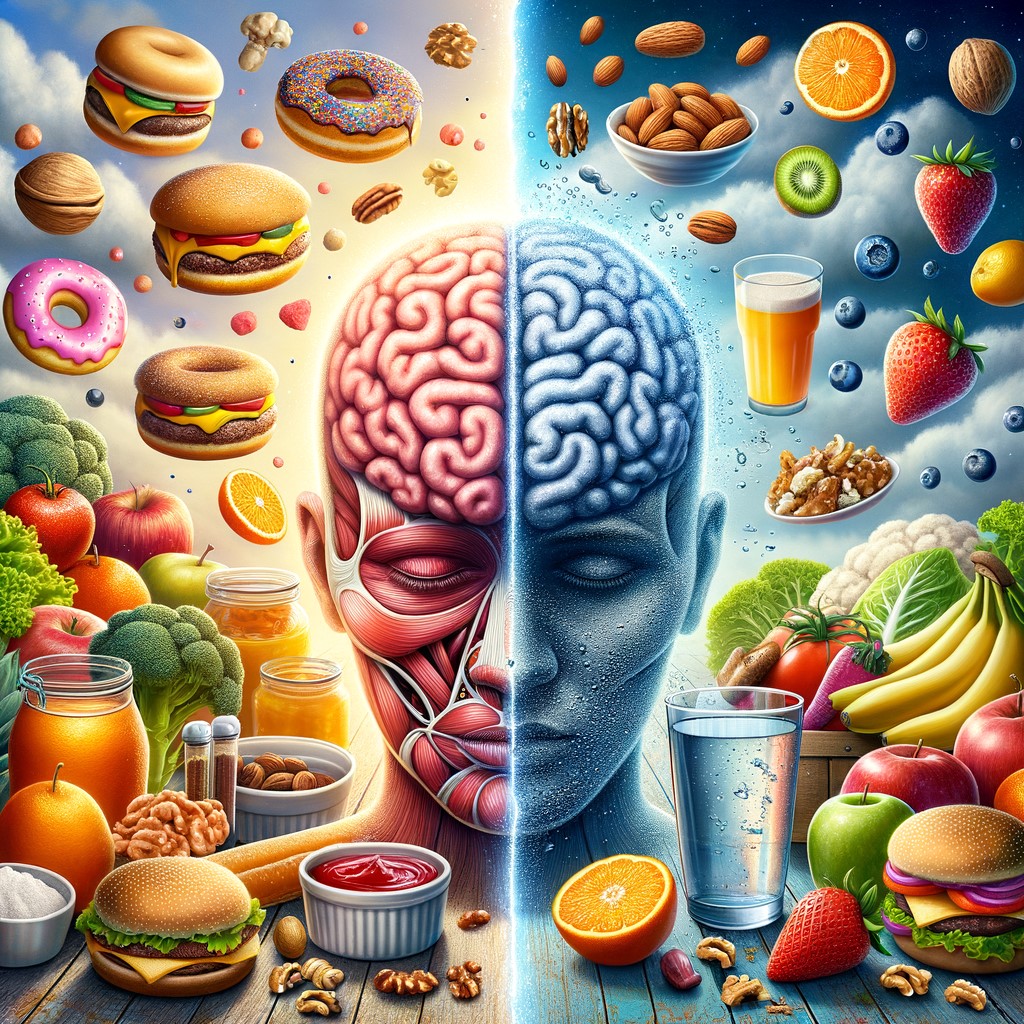
Nutrition is often viewed primarily through the lens of physical health, yet its profound influence on mental clarity and cognitive function remains underappreciated. Emerging research highlights a surprising connection between dietary habits, nutritional deficiencies, and cognitive disorders such as delirium and dementia.
From understanding how poor nutrition can lead to confusion to exploring the impact of early satiety associated with certain cancers, this article delves into the critical role that diet plays in maintaining optimal brain function. By examining specific nutrient deficiencies associated with altered mental states and behavioral changes, we gain valuable insights into preventive strategies that aim to safeguard our cognitive health.
GreatLife Isn’t Just a Program—It’s Your Launchpad to Lasting Success.
1. Understanding How Poor Nutrition Can Lead to Confusion
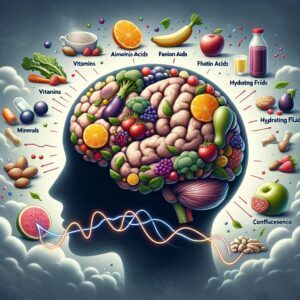
Nutrition plays a critical role in maintaining optimal cognitive function, and poor dietary habits can significantly impair mental clarity, leading to confusion and diminished cognitive performance. The brain requires a consistent supply of essential nutrients, including glucose, vitamins, minerals, amino acids, and fatty acids, to function effectively. When the diet lacks these vital components or is excessively high in processed foods and sugars, it disrupts the balance of neurotransmitters and impairs neural communication pathways.
One primary mechanism by which inadequate nutrition contributes to confusion involves fluctuations in blood sugar levels. Diets high in refined carbohydrates cause rapid spikes followed by sharp declines in blood glucose levels—commonly referred to as hypoglycemia—which can lead directly to symptoms like dizziness, difficulty concentrating, irritability, and mental fogginess.
Additionally, chronic nutritional deficiencies of key vitamins, such as B-complex vitamins (particularly vitamin B12), vitamin D, iron, magnesium, omega-3 fatty acids, and antioxidants, have been shown through research studies to negatively impact memory retention capabilities while increasing susceptibility to cognitive impairment.
Furthermore, dehydration—a common consequence of insufficient fluid intake—is another nutritional factor closely linked with impaired cognition. Even mild dehydration has been clinically demonstrated to significantly reduce attention span, while also causing increased feelings of fatigue or disorientation among individuals across various age groups.
Tired of the same old routine? Break free at Great Life Worldwide! Discover its exciting opportunities and take a free tour now.
2. Nutritional Deficiencies That Commonly Trigger Delirium
Delirium, characterized by sudden confusion and altered mental states, is frequently linked to specific nutritional deficiencies that compromise cognitive function. Among the most common culprits are deficiencies in vitamin B12, thiamine (vitamin B1), folate, and electrolytes such as sodium and potassium.
Vitamin B12 deficiency is particularly prevalent among older adults due to decreased absorption capacity with age or dietary restrictions, such as vegetarianism or veganism, without proper supplementation. This deficiency can lead to neurological impairments manifesting as confusion, memory loss, disorientation, and even hallucinations.
Thiamine deficiency also significantly contributes to delirium symptoms, as it plays a crucial role in glucose metabolism within brain cells. Without adequate thiamine levels—often seen in chronic alcohol users or individuals suffering from severe malnutrition—the brain’s energy production becomes compromised, resulting in acute cognitive dysfunction known as Wernicke’s encephalopathy. Similarly, insufficient folate intake has been linked to impaired neurotransmitter synthesis, which can impact mood regulation and cognitive function.
Electrolyte imbalances further exacerbate delirious episodes by disrupting neuronal signaling pathways critical for maintaining transparent thought processes. Hyponatremia (low sodium) commonly occurs due to dehydration or certain medications like diuretics; this imbalance can rapidly induce confusion and lethargy if left untreated. Likewise, hypokalemia (low potassium) negatively impacts nerve conduction efficiency, leading directly to impaired consciousness levels.
Recognizing these nutritional deficits early allows healthcare professionals an opportunity for prompt intervention through targeted dietary adjustments or supplementation strategies aimed at restoring optimal nutrient balance quickly, thus mitigating risks associated with prolonged periods of delirium-induced cognitive decline.

Take Control of Your Wellness and Wealth—Start Your GreatLife Today.
3. Exploring the Connection Between Malnutrition and Dementia Symptoms
Emerging research has increasingly highlighted a significant correlation between malnutrition and the exacerbation of dementia symptoms. Malnutrition, characterized by inadequate intake or absorption of essential nutrients, can profoundly impact cognitive function, memory retention, and overall mental clarity in individuals already predisposed to dementia or cognitive decline.
One critical aspect of this connection involves deficiencies in key vitamins and minerals such as vitamin B12, folate, omega-3 fatty acids, and antioxidants like vitamins C and E. Deficiencies in these nutrients have been linked to increased oxidative stress within brain cells, inflammation throughout neural pathways, impaired neurotransmitter synthesis, and accelerated neuronal degeneration—all factors known to worsen dementia-related symptoms.
Additionally, protein-energy malnutrition (PEM), commonly observed among elderly populations due to reduced appetite or difficulty eating independently, further complicates cognitive health. PEM contributes directly to muscle wasting, including loss of lean body mass, which negatively affects physical strength and mobility. This deterioration often leads to decreased independence in daily activities that stimulate cognition—such as social interaction or engaging hobbies—thus indirectly accelerating cognitive decline.
Moreover, chronic malnutrition can lead to metabolic disturbances that impair glucose regulation within the brain, a crucial factor since adequate glucose metabolism is vital for optimal neurological functioning. When compromised by poor nutrition over extended periods, these metabolic disruptions may accelerate existing neuropathological processes associated with Alzheimer’s disease or other forms of dementia.
Addressing nutritional status through early intervention strategies such as dietary modifications tailored specifically toward nutrient-rich foods has demonstrated potential benefits in slowing symptom progression while enhancing quality-of-life outcomes for patients experiencing dementia-related conditions.
4. Identifying the Leading Cause of Dementia: Is Diet a Factor?
Emerging research increasingly highlights diet as a significant factor influencing dementia risk, alongside genetics and lifestyle choices. While Alzheimer’s disease remains the most common form of dementia, vascular dementia—often linked to cardiovascular health—is also prevalent. Studies indicate that dietary patterns rich in saturated fats, refined sugars, and processed foods can negatively impact cognitive function by promoting inflammation and oxidative stress within brain tissues.
Conversely, diets emphasizing nutrient-dense foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats, have been associated with a reduced risk of cognitive decline. The Mediterranean diet is frequently cited for its protective effects against dementia due to its high content of antioxidants and anti-inflammatory compounds found in olive oil, nuts, fish rich in omega-3 fatty acids (such as salmon), berries high in flavonoids (like blueberries), leafy greens abundant in folate and vitamin K (spinach or kale), and legumes providing fiber.
Additionally, nutritional deficiencies—particularly vitamins B12 and D—have been directly correlated with increased susceptibility to cognitive impairment. Vitamin B12 deficiency can lead to neurological damage manifesting as memory loss or confusion; similarly, inadequate vitamin D levels are linked with accelerated cognitive decline among older adults.
Therefore, while no single dietary component alone definitively causes or prevents dementia entirely on its merit, yet identified scientifically thus far, the cumulative evidence strongly supports nutrition playing an influential role, either exacerbating vulnerability towards developing dementias through poor dietary habits, or conversely, mitigating risk via consistent adherence to healthier eating practices over time.

Dreaming of a better life? Make it a reality! Visit Great Life Worldwide to explore the fantastic opportunities. Take the free tour today!
5. Early Satiety and Weight Gain: Could Eating Too Little Be Harmful?
Early satiety, characterized by feeling full after consuming only small amounts of food, can significantly impact nutritional intake and overall health. While it may seem counterintuitive, eating too little due to early satiety can lead to unintended weight gain and negatively affect cognitive function.
When individuals consistently consume inadequate calories or nutrients because they feel prematurely satisfied during meals, their bodies often respond by slowing metabolism as a protective mechanism against perceived starvation. This metabolic slowdown makes it easier for the body to store fat from even minimal caloric intake, resulting in unexpected weight gain despite reduced food consumption.
Moreover, insufficient nutrient intake stemming from early satiety can impair cognitive performance and mental clarity over time. Essential vitamins and minerals, such as vitamin B12, iron, zinc, omega-3 fatty acids, and antioxidants, play critical roles in maintaining optimal brain function. Deficiencies in these nutrients are associated with decreased concentration levels, memory impairment, mood disturbances, including symptoms of depression or anxiety, and diminished executive functioning skills.
Additionally, chronic undernutrition caused by persistent early fullness may exacerbate existing medical conditions that further compromise cognitive health, such as diabetes mellitus or cardiovascular disease, by disrupting blood sugar regulation or circulation patterns necessary for proper brain activity. Healthcare professionals emphasize addressing the underlying causes of early satiety promptly through comprehensive assessments, including gastrointestinal evaluations, alongside dietary interventions tailored specifically toward improving caloric density without overwhelming digestive capacity.
Thus, recognizing how eating too little due to premature feelings of fullness affects both physical well-being through unintended weight fluctuations, as well as cognitive abilities, underscores the importance of proactive nutritional management strategies aimed at restoring balanced meal consumption habits essential for sustained mental clarity throughout life stages.
Ready for a Life Upgrade? GreatLife Has the Tools—You Bring the Will.
6. Cancers Associated with Early Satiety and Their Impact on Nutrition
Early satiety, characterized by feeling full after consuming only small amounts of food, can be an important clinical indicator associated with certain cancers. Malignancies such as gastric cancer, pancreatic cancer, ovarian cancer, and liver tumors frequently present early satiety as a symptom due to their anatomical location or physiological impact on the digestive system. These cancers often exert pressure or obstruction within the gastrointestinal tract or abdominal cavity, significantly reducing stomach capacity and altering normal digestion processes.
The presence of early satiety in patients suffering from these malignancies poses substantial nutritional challenges. Reduced food intake leads to inadequate caloric intake and nutrient deficiencies, which negatively affect overall health status. Patients experiencing persistent early fullness may unintentionally limit their dietary variety and volume, resulting in weight loss, muscle wasting (cachexia), fatigue, impaired immune function, and diminished quality of life.
Moreover, compromised nutrition stemming from prolonged early satiety can adversely influence treatment outcomes for oncology patients. Chemotherapy regimens require adequate nutritional support to maintain patient strength and resilience; thus, malnutrition can hinder therapeutic effectiveness while increasing susceptibility to complications during treatment cycles.
Healthcare professionals must remain vigilant when evaluating individuals presenting with unexplained early satiety symptoms, particularly in older adults or those at higher risk, to promptly identify underlying malignancies that impact nutritional status. Timely diagnosis enables clinicians to implement targeted interventions that improve dietary intake through specialized nutrition plans or supplemental feeding strategies tailored to manage symptoms directly related to tumor burden.
Addressing the complex interplay between cancer-induced early satiety symptoms and subsequent nutritional deterioration is essential for optimizing patient care outcomes across multidisciplinary oncology teams.
7. Behavioral Changes and Altered Mental Status Linked to Nutritional Imbalances
Nutritional imbalances can significantly impact mental status, manifesting as behavioral changes ranging from mild irritability to severe cognitive impairment. Deficiencies in essential nutrients, such as vitamin B12, folate, magnesium, and omega-3 fatty acids, have been closely linked to alterations in mood, behavior, and overall cognitive function. For instance, insufficient levels of vitamin B12 are frequently associated with symptoms including confusion, memory loss, depression, anxiety disorders, and even psychosis if left untreated.
Similarly, low magnesium levels can trigger increased agitation or restlessness due to its critical role in regulating neurotransmitter activity within the brain. Omega-3 fatty acid deficiencies may also contribute to emotional instability and impaired decision-making capabilities by negatively affecting neuronal membrane integrity and synaptic plasticity.
Conversely, excess intake of specific nutrients can equally disrupt mental clarity; elevated sodium consumption has been shown to cause neurological disturbances such as confusion or lethargy through electrolyte imbalance-induced cerebral edema. Additionally, drastic fluctuations in blood glucose levels resulting from poor dietary habits may lead directly to altered consciousness states characterized by irritability or difficulty concentrating.
Recognizing these behavioral shifts early is crucial for prompt intervention through nutritional adjustments that aim to restore balance. Healthcare professionals should carefully evaluate dietary patterns when patients present with unexplained changes in cognition or personality traits, especially in the absence of a precise psychiatric diagnosis. Comprehensive nutritional assessments, combined with targeted supplementation strategies, offer an effective means for reversing many nutritionally induced behavioral abnormalities while promoting sustained cognitive health over time.
Dreaming of a better life? Make it a reality! Visit Great Life Worldwide to explore the fantastic opportunities. Take the free tour today!
Conclusion:
The intricate relationship between nutrition, mental clarity, and cognitive health underscores the importance of mindful eating practices throughout all stages of life. Nutritional imbalances—whether due to inadequate intake or underlying medical conditions—can significantly impair cognition by triggering symptoms ranging from mild confusion to severe delirium or dementia-like manifestations.
Recognizing these connections allows healthcare professionals and individuals alike to proactively address dietary concerns before they escalate into serious neurological complications. Ultimately, prioritizing balanced meals rich in essential vitamins, minerals, healthy fats, proteins—and ensuring adequate hydration—is fundamental not only for physical well-being but also for preserving clear thinking abilities crucial for overall quality-of-life outcomes.