In this comprehensive guide, we embark on a journey to demystify pain relief by exploring the spectrum of strong painkillers—from understanding their types, mechanisms, and potency to contrasting prescription options with over-the-counter solutions.
The article delves into the roles of specific medications like tramadol and gabapentin, compares modern alternatives to morphine, and emphasizes safety concerns, particularly for long-term use and kidney health.
With insights on rapid-relief solutions and the importance of tailoring pain management to individual needs, the content equips readers with the knowledge to make informed decisions and set realistic expectations in their pursuit of effective pain management.
Nourish Your Body, Fuel Your Potential—Start with GreatLife Supplements.
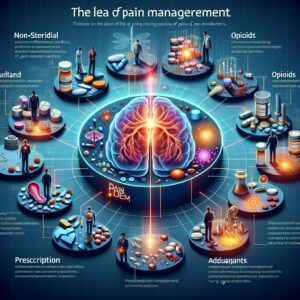
1. Understanding Painkillers: Types, Mechanisms, and Potency
Painkillers play a crucial role in managing various pain conditions, providing relief and improving the quality of life for many patients. These medications are broadly categorized into several groups, including non-steroidal anti-inflammatory drugs (NSAIDs), opioids, and adjuvants, each distinguished by unique mechanisms of action and varying levels of potency.
NSAIDs work by inhibiting cyclooxygenase enzymes, which are critical in the production of inflammatory mediators responsible for pain. This mechanism makes them particularly effective for mild to moderate discomfort while posing a lower risk for dependency.
Opioids, in contrast, bind to specific receptors within the central nervous system, modulating pain perception and providing significant relief in cases of severe pain. However, due to their high potency, opioids require careful oversight to avoid potential adverse effects and dependency issues.
Adjuvant agents such as certain anticonvulsants and antidepressants also play a significant role in pain management, particularly in addressing neuropathic pain. By targeting nerve signal transmission, these drugs provide valuable support when traditional analgesics prove insufficient. Understanding the pharmacodynamics and pharmacokinetics of these pain-relieving medications is integral for prescribing the correct treatment strategy.
Clinicians assess numerous factors, including the underlying cause of pain, patient history, and the specific action of each medication, to ensure the most effective and safest therapeutic approach. Continuous advancements in medical research further illuminate the complexities of pain modulation, paving the way for innovative treatments and refined pain management protocols.
Through this detailed understanding of types, mechanisms, and potency, healthcare professionals can better navigate the challenges presented by pain, ultimately improving patient outcomes.
A comprehensive grasp of these pharmacological principles enables practitioners to customize pain management regimens effectively, ensuring both immediate relief and long-term safety. Ongoing education and research remain essential to address emerging challenges in pain therapy while safeguarding patient well-being. This integration fosters superior clinical outcomes.

Support Your Immune System Naturally—Explore Our Health Essentials Today.
2. Prescription vs. Over-the-Counter: What’s Available and When?
Navigating the differences between prescription and over-the-counter (OTC) painkillers is essential for safe and effective pain management. Prescription painkillers are typically reserved for managing moderate to severe pain that demands targeted intervention.
These medications, including opioids and specific anti-inflammatory agents, are available only when overseen by a licensed healthcare provider. Their use involves careful assessment of individual patient history, potential allergies, and interactions with other medications, ensuring a tailored treatment plan that maximizes benefits while limiting risks.
In contrast, over-the-counter pain relievers are readily available without a prescription and are typically intended for managing mild to moderate discomfort. Common examples include nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen.
Although these medications are generally considered safe when used as directed, they remain subject to guidelines regarding dosage and duration of use. Consumers should strictly adhere to label instructions to minimize risks, such as gastrointestinal complications or other side effects.
Effective decision-making in pain management relies on understanding the clinical context and severity of symptoms. For acute pain episodes or chronic conditions, healthcare professionals may opt for prescription formulations that offer more robust efficacy.
Meanwhile, OTC options provide convenience and accessibility for everyday aches or mild injuries. It is crucial to note that escalating pain indicators should prompt consultation with a medical provider rather than self-medicating with higher doses of OTC products.
Both prescription and OTC painkillers have distinct roles in managing pain. Strategic selection, guided by professional advice, ensures that treatment corresponds to the specific needs and medical circumstances of the patient. Such an approach ultimately fosters improved outcomes, ensuring proper usage and vigilance regarding potential side effects.
In summary, understanding the clear distinctions between prescription and OTC painkillers equips patients and practitioners with critical insights for optimal pain management. This informed approach supports both efficacy and patient safety by carefully selecting medications.
Say Goodbye to Fatigue—Feel the GreatLife Energy Difference.
3. Spotlight on Tramadol and Gabapentin: Evaluating Their Strength and Role
Tramadol and gabapentin have emerged as noteworthy options in the spectrum of pain management, each offering distinct pharmacological profiles that warrant careful evaluation. Tramadol, classified as a synthetic opioid analgesic, functions by binding to opioid receptors and inhibiting the reuptake of norepinephrine and serotonin.
This dual mechanism not only delivers moderate analgesic effects but also makes it an effective option for treating moderate to moderately severe pain. Its utility is particularly evident in cases where traditional non-opioid medications fall short, though its use requires vigilant monitoring due to potential side effects and dependency risks.
In contrast, gabapentin, initially developed for managing neuropathic pain and seizure disorders, operates through modulation of voltage-gated calcium channels. Its mechanism of action does not confer typical opioid-related effects, making it a valuable alternative when addressing pain with a neuropathic component.
Gabapentin is frequently utilized in scenarios where patients present with chronic pain syndromes, and its safety profile, though generally favorable, necessitates dosage adjustment based on individual tolerance and renal function.
When evaluating the strength and overall role of healthcare providers, they must consider factors such as pain etiology, patient history, and the presence of comorbid conditions. Tramadol’s moderate opioid properties render it a viable candidate for cases that require a balance between efficacy and safety when compared with more potent opioids.
Meanwhile, gabapentin fills a critical niche by addressing pain that is less responsive to conventional analgesics, particularly when nerve involvement is suspected. Both medications require a thoughtful assessment of risks and benefits, and their selection should be based on an individualized treatment plan that adapts to the patient’s evolving needs while maintaining a focus on optimal pain management and quality of life.
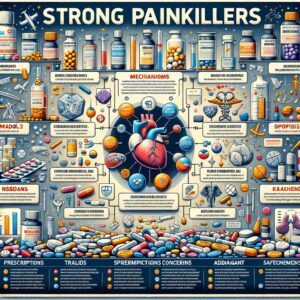
4. Beyond Morphine: Comparing Painkillers in Terms of Efficacy
Comparing painkillers beyond the traditional benchmark of morphine requires an in-depth understanding of pharmacodynamics, patient variability, and evolving clinical protocols. Clinicians assess efficacy by evaluating receptor binding affinity, onset speed, duration of action, and side effect profiles.
While morphine remains a standard, alternatives such as hydromorphone, fentanyl, oxycodone, and non-opioid analgesics provide diverse options tailored to specific pain scenarios. Each agent demonstrates distinct characteristics; for instance, hydromorphone may achieve similar analgesia at lower doses, whereas fentanyl offers rapid relief for acute settings.
It’s essential to acknowledge that efficacy studies now encompass more than just pain intensity reduction. Modern evaluations include quality of life improvements, functional restoration, and patient-reported outcomes.
Recent research supports integrating multimodal analgesia approaches that combine opioids with adjuvant therapies such as antidepressants, anticonvulsants, or muscle relaxants. Such combinations can enhance overall pain management while limiting the dosage and potential adverse effects of any single medication.
Furthermore, individual factors, including metabolic rate, genetic predisposition, and previous treatment responses, significantly influence the performance of painkillers. In practice, a tailored approach that considers these factors is essential. Comparative analyses of painkillers must therefore strike a balance between robust analgesic potential and patient safety and long-term health outcomes.
Advanced clinical trials continue to refine our understanding of efficacy by incorporating biomarkers and predictive models, thereby enhancing our understanding of disease progression and treatment outcomes. As these methodologies advance, they promise to offer more precise guidelines that will ultimately supplant generic comparisons in favor of highly individualized pain management strategies.
Emerging evidence continues to shed light on how dosing regimens, delivery systems, and combination therapies maximize analgesic efficacy while mitigating risks. Clinicians are increasingly relying on comparative studies to guide evidence-based and patient-centric treatment pathways.
Such data-driven approaches ensure that the chosen painkiller not only delivers prompt, effective relief but also aligns with individual therapeutic needs, establishing a comprehensive framework for modern pain management.
Take Charge of Your Health—One Supplement at a Time.
5. Safety First: Long-Term Use and Kidney-Friendly Options
Ensuring safety is paramount when considering long-term use of strong painkillers. Medical professionals emphasize that a thoughtful assessment of both efficacy and potential adverse effects is essential, particularly regarding kidney health. Prolonged use of certain analgesics can pose risks to renal function, especially among individuals with pre-existing conditions. Therefore, vigilant monitoring and routine kidney function tests are crucial under any extended pain management plan.
For those requiring continuous pain management, a shift towards kidney-friendly options can offer a balanced approach to addressing pain while minimizing adverse renal impact. Clinicians are increasingly exploring therapies that reduce reliance on non-steroidal anti-inflammatory drugs known to contribute to kidney strain in chronic settings.
Instead, a combination of alternative medications, adjusted dosages, and intermittent use is often recommended. Furthermore, individualized treatment strategies can include a comprehensive review of the patient’s overall health profile, with particular attention to hydration, blood pressure management, and any indicators of renal distress.
Equally important is adherence to precise dosing regimens and regular consultations with healthcare providers to ensure optimal therapeutic outcomes. Prevention of kidney-related issues involves not only selecting the most appropriate pharmacologic agents but also integrating lifestyle modifications, such as dietary adjustments and exercise, that support renal health.
Educating patients about the signs of kidney stress and the importance of prompt reporting can foster an environment of proactive care. Ultimately, the quest for effective pain management requires a strategic balance between symptomatic relief and the preservation of long-term kidney function, ensuring that safety remains paramount in therapeutic decision-making.
Current research is pivotal in identifying alternative therapies that minimize renal strain while delivering effective pain relief. Evidence supports the thoughtful application of updated dosing strategies and patient monitoring protocols, thereby empowering clinicians to optimize treatment plans for those requiring long-term pain management. This progress enhances overall patient safety.
Unlock Peak Performance—Personalized Nutrition Starts Here.
6. Fast-Acting Solutions: Exploring Rapid-Relief Painkillers
Rapid-relief painkillers represent a pivotal component in managing acute pain by delivering prompt alleviation when immediate intervention is critical. These agents are engineered for a swift onset of action, effectively interrupting pain signals and providing timely control in cases such as postoperative discomfort, acute injuries, and severe breakthrough episodes.
Their formulations are optimized for rapid absorption, ensuring that active compounds reach therapeutic levels quickly in the bloodstream. Diverse delivery systems, including fast-dissolving oral tablets, intravenous injections, and transdermal patches, have been developed to address various clinical scenarios.
Healthcare professionals utilize these options to tailor pain management strategies to meet the specific needs of each patient, taking into account the severity of their pain and any associated medical conditions. The pharmacokinetic profiles of rapid-acting painkillers are extensively evaluated during clinical studies to confirm their efficacy and safety.
Regulatory agencies impose rigorous standards to ensure quality, ensuring that these medications provide consistent and immediate relief while minimizing risks such as dependency and adverse reactions. In addition to prompt pain mitigation, the use of fast-acting formulations plays a critical role in improving overall patient care by reducing agitation and facilitating quicker recovery times in acute settings.
Furthermore, advancements in pharmaceutical technology continue to enhance the performance of these medications. Emerging formulations focus on increasing bioavailability and minimizing delay in therapeutic effect, thereby offering a more reliable response for patients in urgent need. Clinicians must assess individual patient profiles, considering potential drug interactions and existing health conditions, to determine the most appropriate rapid-relief option.
Ultimately, fast-acting painkillers significantly contribute to effective pain management, supporting both immediate symptom relief and improved patient outcomes in various acute care settings. These rapid-relief formulations not only address immediate discomfort but also provide critical support in dynamic clinical environments, enabling healthcare teams to deliver targeted interventions that consistently optimize pain control and contribute to enhanced overall treatment efficacy.
7. Making Informed Choices: Matching Painkiller Strength to Individual Needs
When choosing a painkiller, it is essential to adopt a measured, informed approach that considers both effectiveness and individual tolerance. A thorough evaluation of the patient’s unique pain profile, medical history, and lifestyle is crucial in selecting the most suitable medication.
Clinicians must balance the potential benefits of substantial pain relief against possible risks, including side effects, dependency issues, and interactions with other treatments. For individuals with mild pain, over-the-counter alternatives or lower potency medications may suffice, whereas patients experiencing severe or chronic pain might require medications with higher analgesic strength under careful supervision.
A detailed assessment of factors such as age, kidney and liver function, and previous responses to pain management regimens is indispensable. In tailoring pain management strategies, open dialogue between patients and healthcare providers is crucial for understanding personal preferences and managing expectations.
This collaborative process ensures that treatment plans are both safe and effective, tailoring them to the nuances of each case. Furthermore, periodic reviews of the patient’s response to medication help fine-tune dosages and switch to more suitable alternatives when necessary.
Leveraging both clinical expertise and patient input, medical professionals can customize pain management in a way that aligns with each patient’s specific needs. By integrating current research findings with personalized care strategies, the prescription of painkillers is optimized to provide maximum relief while minimizing adverse outcomes. Ultimately, a tailored approach not only improves the immediate quality of life but also promotes long-term well-being by reducing the risks associated with inappropriate painkiller use.
Advances in pharmacology and patient care continue to refine effective pain management. Staying informed and engaging in ongoing dialogue with healthcare providers fosters a personalized treatment plan that supports overall well-being, ensuring that pain relief strategies evolve to meet changing needs and optimize patient outcomes. Continuous reassessment remains vital for achieving optimal results.

Your Health Journey Deserves the Best—Choose GreatLife Quality.
Conclusion:
Ultimately, the exploration of diverse painkillers illustrates that effective pain management requires a careful balance between potency, safety, and individualized treatment strategies. By critically examining various medications, their mechanisms, and the key differences between prescription and over-the-counter (OTC) options, the guide reinforces the importance of maintaining continuous dialogue with healthcare professionals. As medical advancements shape the future landscape of pain relief, the emphasis remains on making informed choices that prioritize both immediate comfort and long-term well-being.

